When a tooth is badly impacted or broken, sometimes a standard extraction isn’t enough to remove the tooth entirely. This is where surgical tooth removal comes in. Surgical extractions sound intimidating, but they are common procedures that can save you from ongoing pain and infection. In this blog, we’ll explain what surgical tooth removal involves, when it’s needed, and how we at Vallance Dental Centre ensure your comfort and safety every step of the way.
What is a Surgical Extraction and When Do You Need One?
A surgical tooth extraction is a procedure to remove a tooth that cannot be easily accessed or removed with simple techniques. In a simple extraction, a dentist can grasp the visible part of a tooth and pull it out using forceps. In contrast, a surgical extraction is often required when the tooth is not fully visible or is otherwise difficult to remove. This may be the case if:
-
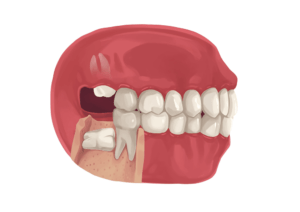
The tooth is impacted – for example, a wisdom tooth that is stuck under the gum or bone, or a tooth that is pressing against the adjacent tooth at an angle.
-
The tooth has broken off at the gum line (leaving no crown to grab onto), often due to decay or trauma (colgate.com)
-
The roots are abnormally long or curved, or the tooth has multiple roots that make it firmly anchored.
-
There is dense bone or other obstacles around the tooth. Sometimes overgrown tissue or a small bit of bone needs removal to free the tooth
-
The tooth is a wisdom tooth (third molar) that hasn’t fully erupted. Wisdom teeth are the most frequent candidates for surgical extraction, especially if they are coming in sideways or only partially through the gum
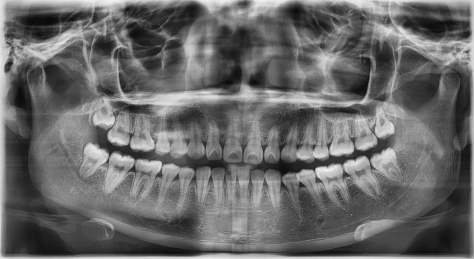
In short, surgical removal is needed when simple removal is not possible or could risk damage to surrounding areas. Your dentist will determine this from X-rays and exam. At our clinic, we take a careful assessment – if we see, for instance, a horizontal wisdom tooth or a retained root tip under the gum, we’ll plan a surgical approach from the start.
Don’t be alarmed by the term “surgical.” It basically means the dentist will make a small incision in the gum and possibly remove a bit of bone to get the tooth out, rather than just pulling it. It’s a routine oral surgery procedure, typically done under local anesthesia in the dental office. In rare cases (such as multiple impacted wisdom teeth or complex cases), surgical extractions might be done under IV sedation or general anesthesia – we would discuss the best setting for your situation. But the vast majority of surgical removals, even of wisdom teeth, are safely done right here at Vallance Dental Centre with local numbing and perhaps an oral sedative prescription for anxiety.
How Does Surgical Tooth Removal Differ from a Simple Extraction?
The main differences boil down to the technique and sometimes the extent of tissue involved:
-
Incision and Access: In a surgical extraction, the gum tissue covering the tooth will be opened with a small incision to expose the tooth or its roots. In some cases, a tiny portion of bone covering the tooth may be removed with a drill to gain access. None of this is done in a simple extraction, where the tooth is fully visible.
-
Sectioning the Tooth: Often in surgical extractions, the dentist will divide the tooth into sections. For example, cutting a molar into halves or thirds allows removal in pieces rather than one entire chunk. This is gentler on the surrounding bone and helps remove the tooth through a smaller opening. Simple extractions remove the tooth whole.
-
Stitches: Surgical extractions usually require stitches (sutures) afterwards to close the gum tissue that was opened. These stitches are typically dissolvable and aid healing. In a simple extraction, no stitches are needed because the gum wasn’t cut.
-
Duration: A surgical extraction can take longer than a simple one. A straightforward simple extraction might be done in 10 minutes, whereas a surgical removal might take 30–45 minutes (sometimes longer for complicated wisdom teeth). This is because of the extra steps (incising, bone removal, sectioning, suturing). Despite taking longer, the procedure is done with great care to minimise trauma.
-
Complexity and Personnel: A general dentist can perform many surgical extractions. However, if a case is very complex or requires deep sedation, an oral surgeon might handle it. At Vallance Dental Centre, our dentists handle most surgical extractions in-house, but we work with two dentists who have extensive surgical experience for challenging cases.
-
Recovery: Surgical removals generally have a bit more post-op swelling and a slightly longer healing time compared to simple extractions, given the minor surgery to the gums/bone. We’ll cover recovery details below, but expect perhaps a couple of extra days of healing time for a surgical site.
Despite these differences, the goal is the same: to remove the problematic tooth safely and relieve your symptoms. We tailor the approach to what’s best for you. Our team will explain if your tooth needs a surgical approach and why, so you’re fully informed.
Step-by-Step: How a Surgical Extraction Procedure Works
Knowing what will happen during a surgical extraction can ease a lot of anxiety. Here’s a step-by-step breakdown of a typical surgical tooth removal at our clinic:
-
1. Numbing the Area:
We begin by administering local anesthetic, just as we would for a filling or simple extraction. The numbing process involves a small injection (with topical numbing gel pre-applied so you barely feel the pinch). We ensure the entire area – tooth, surrounding gum, and bone – is completely numb. You might feel your tongue or lip getting fat and tingly. We test the area thoroughly before starting. (If you’re nervous, we can discuss dental sedation options such as IV sedation or oral medication to help you relax during this step and throughout the procedure.
-
2. Accessing the Tooth
Once numb, the dentist makes a small incision in the gum tissue over the tooth. If a flap of gum is covering an impacted tooth, this incision allows it to be folded back (like opening a tiny curtain) to reveal the tooth underneath. Occasionally, a bit of the bone that still blocks the tooth may be removed using a handheld drill – you’d feel vibration but no pain. Just like a filling. This creates a direct path to the tooth. Don’t worry, removing that small amount of bone will not harm you; it heals later, and this step is only done if absolutely necessary.
-
3. Sectioning (if needed)
If the tooth is large or awkwardly positioned, the dentist will cut the tooth into sections using a surgical handpiece. For instance, a wisdom tooth might be sectioned into halves or thirds. This sounds dramatic, but it’s actually a very controlled technique that makes removal gentler. By sectioning, each piece can be taken out more easily without tugging excessively on your jaw. You might hear a high-pitched sound during this process (from the drill) and feel vibration, but remember you’re numb – you should feel no sharp pain. We also irrigate with water to keep the area cool and clear.
-
4. Removing the Tooth
Using specialized instruments (small elevators and forceps), the dentist will carefully remove each section of the tooth. You will feel pressure as the pieces are pried or lifted out – the pressure comes from the dentist working the tooth loose. This step can involve some firm pushing, but since the area is numb you’ll feel the sensation without pain. If at any point you’re uncomfortable, we can pause and give more numbing. Most patients say it’s odd but not painful. The tooth pieces are removed one by one until the entire tooth is out.
-
5. After Removal – Cleaning the Site
Once the tooth is gone, we will thoroughly clean the now-empty socket. Any small debris or bone fragments are suctioned out. If the tooth was infected or there was an abscess, we’ll also ensure that is drained and cleaned. In some cases, we may place a small medicated dressing or a bit of bone graft material if needed (your dentist will discuss if that’s something indicated for you – it’s not common for routine cases, more for planning implants later).
-
6. Suturing (Stitches)
The gum tissue flap is put back into place and sutured (stitched) closed with a few dissolvable stitches. These stitches usually dissolve on their own within about 1–2 weeks. They help reconnect the gum edges and promote faster healing. You might feel the dentist tugging gently as stitches are tied – still no pain, since it’s numb, just a bit of pulling sensation.
-
7. Bite Down on Gauze
We’ll have you bite on a gauze pad over the extraction site to apply pressure and help stop bleeding.we’ll go over your post-op instructions verbally and give you a take-home written guide. Once we check that the bleeding is controlled and you’re feeling okay, you’ll be ready to go home. We advise you to keep pressure for 20 minutes, you are welcome to stay in our practice for this time period.
Throughout the procedure, our surgical team maintains strict sterility and monitoring. If you’re sedated, we keep an eye on your vitals (blood pressure, oxygen, heart rate) continuously. Even under local anesthetic, we watch your comfort level closely – you can raise a hand at any time if you need a break or feel something. A surgical extraction is done at your pace; we do not rush. Expect the whole visit to last perhaps an hour to an hour and a half, including prep and recovery time.
What Are the Risks of Surgical Extractions?
Surgical tooth removal is very safe when performed by experienced hands, but it’s natural to have concerns about potential risks.
By choosing a reputable practice for your surgical extraction, you significantly reduce these risks. Our team has successfully performed countless surgical removals, including tough wisdom teeth, with excellent outcomes. We do a thorough consultation so you understand the risks (and their likelihood) before consenting to the procedure. Your safety is paramount to us, and we have protocols in place to prevent and handle complications.
Here are some common risks and how we mitigate them:
-
Pain or Swelling
Some post-operative pain and swelling are expected with any surgical extraction. This is your body’s normal healing response. Swelling of the cheek or jaw is usually mild to moderate and peaks around 48 hours after surgery, then subsides. We help by advising use of effective pain medication eg. paracetamol and ibuprofen. Cold packs can also be helpful. Most patients report the pain is well-controlled with the medication and improves after the second day. If you follow the post-op instructions, you’ll keep discomfort to a minimum.
-
Dry Socket
As mentioned earlier, dry socket (alveolar osteitis) can occur in ~2-5% of cases, especially lower wisdom teeth. This happens if the blood clot gets dislodged early, exposing the bone, and causes intense dull pain a few days post-extraction. If dry socket does occur, we can treat it promptly by cleaning the socket and placing a special soothing paste – this resolves the pain quickly. Dry sockets are temporary and heal, but we work hard to help you avoid them altogether.
-
Infection
Any time you have minor surgery, there’s a slight risk of infection afterwards. We minimize this risk by maintaining a sterile environment during the extraction. Signs of infection include worsening pain after 3-4 days, swelling getting worse rather than better, or fever. It’s uncommon, but if it happens, contact us and we will get you on antibiotics. Good oral hygiene (gentle rinsing beginning 24 hours after procedure, etc.) and not smoking will greatly reduce infection risk.
-
Bleeding
Some oozing from the extraction site is normal in the first 24 hours. We will ensure bleeding is minimal before you leave. Occasionally, bleeding may restart a few hours later (for instance, if you were to accidentally spit or dislodge the clot). That’s why we tell you to go easy. If you do experience persistent bleeding at home, bite firmly on clean gauze and call us. We can guide you over the phone or have you return to the clinic. Significant bleeding is not common – it’s usually just slight oozing that looks worse than it is when mixed with saliva. Following our instructions (rest, head elevated, avoid disturbing the site) keeps bleeding under control.
-
Nerve Injury
For certain lower teeth (especially wisdom teeth or second molars), the roots can be very close to the inferior alveolar nerve or the lingual nerve. These nerves give feeling to your lower lip, chin, and tongue. In rare cases, during extraction, the nerve may be bruised or compressed, leading to numbness or tingling in those areas. We plan carefully with X-rays or 3D scans to map the nerve’s location relative to the tooth. By using precise techniques (and sometimes a coronectomy – removing the crown but leaving roots near the nerve in place, if deemed safer), we protect the nerve. Nerve injury is rare and in most cases of it, the numbness is temporary, resolving over a few weeks or months. Permanent nerve damage from a dental extraction is very uncommon. We will discuss your specific risk if your tooth is near a nerve canal – and take all precautions to avoid it.
-
Sinus Communication
Upper back teeth (molars) have roots near the sinus cavities. Occasionally, removing an upper molar can leave a small opening between the mouth and the sinus. We check for this. If it occurs, we will place additional stitches or other measures to close it. You might be asked to avoid blowing your nose for a short period to allow it to seal. This complication is not common, but it’s easily managed if it happens.
Recovery Tips for a Smooth Healing
Recovering from a surgical tooth removal is very similar to recovering from any extraction, but you may need to allow a bit of extra time for swelling to go down and the incision to heal.
Remember, everyone heals at their own pace. Younger patients might bounce back very quickly, while older patients or those with health conditions may take a bit longer. By following these guidelines, you’re setting yourself up for a smooth recovery. We will schedule a follow-up visit about a week or two after the surgery to ensure everything is healing well (or we’ll call you to check in). Attending that follow-up is important – even if you feel fine – so we can carefully inspect the site and remove any remaining sutures if needed.
Here are some top recovery tips to ensure a smooth healing process:
-
Follow All Instructions
It may sound obvious, but carefully follow the customized instructions we give you. They cover how to manage bleeding, how and when to take medications, and how to keep the area clean. For example, if we prescribed antibiotics, take the full course as directed to prevent infection.
-
Pain Management
Stay ahead of any pain by taking your pain medication on schedule for the first day or two. Don’t wait until pain is severe. Typically, we recommend ibuprofen (Advil/Nurofen) and paracetamol (acetaminophen) as first-line, as this combination can be very effective for dental surgical pain. If we gave you something stronger, use it as directed, especially before bedtime on the first night. Most patients find they only need the strong painkillers for a day or not at all, switching to ibuprofen thereafter. After 48 hours, many people need only minimal pain relief, if any.
-
Reduce Swelling
Expect some cheek swelling, especially with a wisdom tooth surgery. Apply an ice pack (wrapped in a cloth) to the outside of your face on and off for the first 24 hours – e.g. 15 minutes on, 15 minutes off. This helps minimize swelling and bruising. After the first day, switch to warm moist compresses if you still have swelling, as heat can help at that stage. Keep your head slightly elevated when resting (extra pillow) for the first night; it can prevent swelling from pooling.
-
Oral Hygiene
Starting the day after surgery, rinse very gently with warm salt water after meals and before bed. Mix 1/2 teaspoon of salt in a cup of warm water. This keeps the site clean and soothes the area. Do not spit forcefully – just let the water fall out of your mouth into the sink. Continue gentle salt rinses for at least a week. You can also resume brushing your teeth the next day, but be very careful to avoid the surgical area. Do not disturb the stitches. Keeping your mouth clean will help prevent infection.
-
Diet and Hydration
For the first 24-48 hours, stick to a soft diet and stay hydrated. Drink plenty of fluids (water, cold or lukewarm tea, smoothies). Avoid hot temperature drinks for the first day or two, as heat can dissolve the blood clot and cause bleeding. Good nutrition aids healing, so even if you don’t feel like eating, have soups or meal replacement shakes to get some vitamins and protein in. As the days go on, you can slowly introduce more solid foods – just chew away from the surgical site. Avoid foods that crumble (chips, cookies) or small hard bits (nuts, seeds) for about a week. Most people find they can eat normally on the opposite side of the mouth after a few days.
-
Activity
Rest on the day of your surgery. It’s a great excuse to take it easy, catch up on Netflix, or read. Overexertion can lead to more bleeding or pain. After 24-48 hours, you can resume light activities if you feel up to it. However, avoid heavy lifting or strenuous exercise for at least 3–5 days, as that can increase blood pressure and disrupt the healing site. If you exercise and notice throbbing or bleeding, stop and rest for another day or two.
-
No Smoking or Alcohol
As mentioned earlier, smoking is one of the worst things you can do after any extraction – it delays healing and significantly raises dry socket risk. Avoid smoking for at least 2 days (honestly, the longer the better – 1-2 weeks abstinence is ideal if possible). If you drink alcohol, hold off for a few days as well; alcohol can interfere with healing and pain meds.
-
Watch for Warning Signs
Know what’s normal and what’s not. It’s normal to have swelling, mild to moderate pain, and even some light bleeding or oozing in the first 1-2 days. It’s not normal to have severe pain that painkillers don’t help, persistent heavy bleeding, or signs of infection like pus discharge or fever. If you experience anything concerning – for example, increasing pain around day 3-4 instead of getting better – contact us. We’re here to help and can bring you in for a check-up or provide guidance. Often, a quick intervention (like packing a dry socket) can dramatically improve your comfort.
How We Ensure Your Comfort and Safety at Vallance Dental Centre
Undergoing a surgical extraction can be nerve-wracking, but at Vallance Dental Centre you are in very good hands. Our team is committed to making the experience as comfortable as possible and to take excellent care of you before, during, and after the procedure. Here are some ways we prioritize your comfort and safety:
-
Experienced Professionals
Two of our dental team have advanced training and ample experience in surgical extractions, including wisdom tooth removals. Complex cases are handled with a calm, skilled approach. We perform dozens of surgical extractions each year, so we’re well-versed in the best techniques. If there is any aspect outside our scope, we work with trusted local consultants. But rest assured, for the vast majority of cases, you won’t need to go anywhere else.
-
Comprehensive Evaluation
Safety starts with good planning. Before we take on any surgical extraction, we gather all necessary diagnostics – this could mean taking panoramic X-rays or even a CBCT scan for deeply impacted teeth. We evaluate the shape of your roots, the proximity to nerves or sinuses, and the condition of surrounding bone. By the time the procedure day comes, we have a clear game plan that avoids surprises. We’ll also review your medical history to anticipate any special precautions (for example, if you’re on blood thinners or have a condition like diabetes, we factor that into our prep and aftercare).
-
Anesthesia & Sedation Options
We offer sedation options for nervous patients: Oral sedation which can take the edge off, or Intravenous IV sedation medication for a deeper relaxation. Under sedation, many patients have little memory of the procedure and just “nap” through it. Your vital signs are monitored continuously. This is all done to maximize your comfort and reduce anxiety. You will never be judged for being nervous – it’s completely natural, and we’re here to support you.
-
Aseptic Technique
In terms of safety, our clinic follows strict infection control and aseptic techniques. All instruments are sterilized, we use disposable items where appropriate, and the surgical field is kept clean. Our clinicians wear proper protective gear. The procedure is done in a controlled, sanitized environment to prevent any chance of contamination.
-
State-of-the-Art Equipment
We utilize modern equipment which often means shorter procedure times and less trauma. For instance, our surgical handpieces (drills) are high-tech and water-cooled to prevent overheating tissue. We have specialized extraction instruments that allow us to apply focused force without excess pressure. All these little things add up to a smoother surgery and easier recovery for you.
-
Personalized Care and Communication
One thing patients appreciate is that we explain everything as we go (or stay quiet if you prefer!). Some folks like to know “now I’m doing X, now Y” during the procedure – if that reassures you, we are happy to talk you through it. If you’d rather tune out, we can do that too; we even can play your choice of music in the background. You will never be left wondering what’s happening. We also make sure you’re thoroughly numb and comfortable – we check in frequently like “How are you doing? Doing okay?” You are encouraged to raise a hand or signal if you need a break or feel anything. We never rush. Your procedure will be done at a pace that is comfortable for you.
-
Diligent Aftercare
Our care doesn’t stop when you leave the chair. We will give you detailed written post-op instructions and go over key points verbally. We often call patients the next day to check how you’re feeling – especially for more involved surgeries. Continuity of care means you’re not on your own – we’re overseeing your recovery to ensure it’s on track.
Meet Our Experts

Dr Hareem Hadi
Dr Hareem Hadi graduated in 2013 and is a highly skilled dentist with a special interest in oral surgery. She has completed extensive postgraduate training specifically focused on surgical tooth removal. Dr Hareem is passionate about providing comfortable, patient-focused care.

Dr Arfeen Aslam
Dr Arfeen Aslam graduated in 2008 and brings extensive general dentistry experience. In 2018, he was awarded the Best Young Dentist at the Private Dentistry Awards. Dr Arfeen has considerable expertise in oral surgery, complex surgical procedures, and dental implant placements, ensuring exceptional care and outcomes.
Contact us Today by telephone +47 333 78 901 or email reception@vallancedentalcentre.com reception@vallancedentalcentre.com if you require our surgical extraction services
Surgical tooth removal may sound daunting, but in capable hands it’s a routine and safe procedure that can relieve pain and prevent bigger problems down the road. If you’ve been told you need a surgical extraction – whether it’s a troublesome wisdom tooth or a broken molar – don’t worry. With proper technique, adequate anesthesia, and good post-op care, you’ll be on the mend in no time. At Vallance Dental Centre, we perform surgical extractions with a focus on patient comfort and excellent outcomes. From the initial consultation (where we determine if a surgical approach is needed) through the healing check, we’ve got you covered. You’ll receive warm, personalized attention and the benefit of our expertise with oral surgery. Our Manchester patients often remark that their dreaded procedure turned out to be far easier than expected – and that’s the result we strive for every time. If you have any questions about surgical tooth removal or wish to schedule an evaluation, feel free to reach out to us. We’re here to help you keep your mouth healthy and pain-free, using the safest and most comfortable methods available.


